- 20-Jun-23
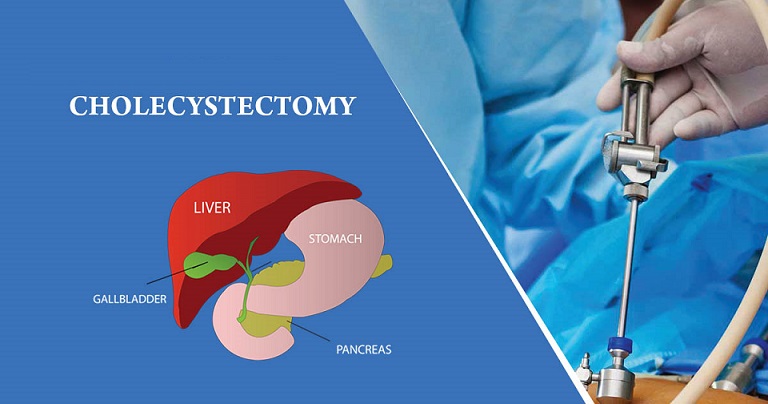
A cholecystectomy is a surgical technique used to remove the gallbladder. The gallbladder is a small organ with a pear-like shape that is situated beneath the liver on the right side of the abdomen. It stores bile, a fluid that facilitates the breakdown of fat. The physician makes a number of tiny incisions in the abdomen and inserts surgical instruments into the incisions to perform a cholecystectomy laparoscopically. A larger abdominal incision may be necessary if an open cholecystectomy is necessary in certain situations.
A cholecystectomy is frequently used to treat gallstones which are solid accumulations in the gallbladder. Gallstones can cause pains, bloating, nausea, vomiting, and these symptoms. They may also have negative effects including cholecystitis, a gallbladder infection, or cholangitis, a gallbladder inflammation. Cholecystectomy is frequently a safe and effective procedure. The likelihood of complications is quite low and the majority of patients are able to go home the day of or the day following surgery.
Types of Cholecystectomy:
There are two main types of cholecystectomy which refer to the surgical removal of the gallbladder:
-
Laparoscopic Cholecystectomy: The most popular and favored method for gallbladder removal is this one. It is a minimally invasive treatment that necessitates numerous tiny abdominal incisions. Through these incisions, specialized equipment and a laparoscope (a narrow tube with a camera) are inserted. The surgeon can use the laparoscope to direct the instruments used to remove the gallbladder while viewing the surgical site on a monitor. In comparison to open cholecystectomy, laparoscopic cholecystectomy frequently produces less pain, shorter hospital stays, and quicker recovery.
-
Open Cholecystectomy: An open cholecystectomy may be performed in some circumstances such as when there are difficulties or when laparoscopic surgery is not possible. It entails creating a solitary, more significant incision in the upper abdomen. The surgeon can directly reach and remove the gallbladder using this incision. Compared to laparoscopic cholecystectomy, open cholecystectomy has a longer recovery time and a higher risk of complications. However, it can be required in complicated circumstances or when there are worries about the laparoscopic approach's safety.
The choice between laparoscopic and open cholecystectomy depends on various factors including the patient's condition, the presence of any complications, the surgeon's expertise, and the patient's individual circumstances. The surgeon will determine the most appropriate approach based on these factors.
Gallbladder Removal Surgery:
The surgeon carefully detaches the gallbladder from the liver and bile ducts and then removes it from the body. After gallbladder removal, bile from the liver flows directly into the small intestine. Recovery from gallbladder removal surgery is typically relatively quick. Most people can resume normal activities within a week or two after laparoscopic cholecystectomy, while recovery from open cholecystectomy may take a bit longer.
It's important to follow the surgeon's post-operative instructions including taking any prescribed medications, caring for the incision sites, and gradually resuming activities as advised. As with any surgical procedure, there are risks involved with gallbladder removal surgery such as infection, bleeding, injury to nearby organs, and complications related to anesthesia. However, these risks are generally low and the benefits of the surgery often outweigh them.
Symptoms of Gallbladder Removal:
After gallbladder removal surgery (cholecystectomy) some people may experience certain symptoms or changes in digestion. These symptoms can vary from person to person and while most individuals do not experience significant issues, some common symptoms after gallbladder removal may include:
- Diarrhea: Some individuals may experience more frequent bowel movements or loose stools after gallbladder removal. This occurs because the gallbladder is responsible for storing and concentrating bile which aids in the digestion of fats. Without the gallbladder, bile flows directly from the liver into the small intestine which can lead to changes in bowel habits.
- Difficulty digesting fatty foods: Without a gallbladder, the body may have a harder time breaking down and digesting fats. This can cause discomfort, bloating, or diarrhea, particularly after consuming foods high in fat.
- Changes in bowel movements: Some individuals may experience changes in the frequency or consistency of their bowel movements. This can range from more frequent or urgent bowel movements to occasional constipation.
- Abdominal pain or discomfort: Some people may experience slight abdominal pain or discomfort for a short while following gallbladder removal surgery despite the fact that the majority of patients recover from the procedure without feeling any significant pain or discomfort. Usually only short-lived, this gets better as your body gets used to it.
It's important to note that not everyone will experience these symptoms and many people can live a normal, healthy life without a gallbladder. If you have concerns or persistent symptoms after gallbladder removal surgery it is recommended to consult with a healthcare professional for further evaluation and guidance. They can provide personalized advice and suggest dietary adjustments or medications to manage any symptoms you may be experiencing.
Best Gastroenterologist in Lahore:
Integrated Medical Care Hospital (IMC Hospital) is one of the most prestigious institutions in Pakistan which is known for its performance and outstanding results regarding Gastroenterology (Stomach Specialist). Here you find one of the Best Gastroenterology (Stomach Diseases) Specialists in Lahore Pakistan. Visit today and book your appointment at Integrated Medical Care Hospital (IMC Hospital).
Prof. Dr. Ghias Un Nabi Tayyab:
MBBS, MRCP (UK), FRCP (Edin), MD (USA), AGAF (USA).
Specialties: Gastroenterology, Hepatology (Liver Diseases).
Dr. Muhammad Bilal Nasir:
MBBS, FCPS(Medicine), FCPS (Gastroenterology), MACG.
Specialties: Gastroenterology.
Dr. Ayesha Hanif Ramay:
MBBS, FCPS (Gastroenterology & Hepatology).
Specialties: Gastroenterology.
Dr. Abdul Qadir:
MBBS, FCPS (Gastroenterology & Hepatology).
Specialties: Gastroenterology.

 Map
Map